# Median Rhomboid Glossitis: Your Comprehensive Guide to Understanding and Managing This Condition
Are you experiencing a smooth, reddish patch on the center of your tongue? You might be dealing with median rhomboid glossitis (MRG). This comprehensive guide provides an in-depth look at MRG, offering expert insights into its causes, symptoms, diagnosis, treatment options, and preventative measures. We aim to equip you with the knowledge you need to understand and manage this condition effectively. This isn’t just another article; it’s a resource built on expertise and a commitment to providing clear, actionable information.
## What is Median Rhomboid Glossitis? A Deep Dive
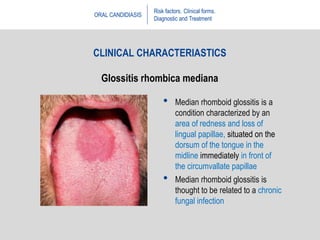
Median rhomboid glossitis, also known as central papillary atrophy, is a benign condition affecting the tongue. It’s characterized by a smooth, often diamond- or rhomboid-shaped, reddish patch located in the midline of the tongue, just in front of the circumvallate papillae. Unlike thrush, it’s typically painless, although some individuals may experience mild discomfort or sensitivity.
Historically, MRG was thought to be a developmental anomaly. However, modern research strongly suggests that it’s primarily associated with chronic *Candida albicans* infection, a type of yeast. The persistent inflammation and altered oral microbiome contribute to the characteristic appearance of the lesion. It’s also worth noting the potential role of other factors such as smoking, dentures, and inhaled corticosteroids, which can create a favorable environment for *Candida* overgrowth.
### Core Concepts and Advanced Principles
At its core, median rhomboid glossitis represents an alteration in the normal tongue surface. The filiform papillae, the small, hair-like projections that give the tongue its texture, are absent in the affected area. This absence results in the smooth, reddish appearance. The underlying inflammation and potential presence of fungal hyphae further contribute to the lesion’s characteristics.
An advanced understanding involves recognizing the interplay between *Candida* infection, local immune response, and predisposing factors. Some individuals may be more susceptible due to underlying health conditions, weakened immune systems, or specific lifestyle habits. Furthermore, the diagnosis often relies on clinical examination, but in some cases, a biopsy may be necessary to rule out other conditions.
### Importance and Current Relevance
While median rhomboid glossitis is generally harmless, it’s important to recognize and manage it for several reasons. First, the visual appearance can be concerning to individuals, leading to anxiety and self-consciousness. Second, the presence of *Candida* overgrowth may indicate an underlying systemic issue or risk for other oral infections. Third, long-term untreated MRG may, in rare cases, lead to secondary bacterial infections or other complications. Recent studies indicate a potential link between chronic oral candidiasis and certain systemic diseases, highlighting the importance of proper diagnosis and management.
## Understanding the Role of Antifungal Medications in Treating MRG
While not a product in itself, the treatment of median rhomboid glossitis often involves the use of antifungal medications. These medications play a crucial role in addressing the underlying *Candida albicans* infection, which is believed to be a primary driver of the condition. Therefore, understanding how antifungal medications work in this context is essential.
From an expert perspective, antifungal medications target the cell walls of fungi, disrupting their ability to grow and reproduce. In the case of MRG, topical antifungal agents like nystatin or clotrimazole are frequently prescribed. These medications are applied directly to the affected area of the tongue, allowing for localized treatment and minimizing systemic side effects. Systemic antifungal medications, such as fluconazole, may be considered in more severe or persistent cases.
## Key Features of Antifungal Medications for Median Rhomboid Glossitis
Here’s a breakdown of key features associated with antifungal medications used to treat median rhomboid glossitis:
1. **Broad Spectrum Activity:** Effective against a range of fungal species, including *Candida albicans*, the most common culprit in MRG.
2. **Topical Application:** Allows for targeted treatment, minimizing systemic absorption and potential side effects. This is generally preferred for MRG.
3. **Various Formulations:** Available in creams, ointments, lozenges, and mouthwashes to suit individual preferences and needs.
4. **Systemic Options:** For severe or resistant cases, oral medications provide a broader approach to fungal eradication.
5. **Minimal Side Effects (Topical):** Topical antifungals generally have few side effects, such as mild irritation or burning at the application site.
6. **Prescription Strength (Systemic):** Systemic antifungals require a prescription due to potential drug interactions and side effects.
7. **Variable Duration of Treatment:** Treatment duration depends on the severity of the infection and the individual’s response, typically ranging from 1-4 weeks.
For each of these features, it is important to understand their impact. For example, broad spectrum activity ensures that the medication can effectively target the specific fungus causing the infection. Topical application minimizes the risk of systemic side effects, making it a safer option for many patients. Different formulations provide flexibility in how the medication is administered, allowing for personalized treatment. The availability of systemic options ensures that more severe or resistant cases can be effectively managed. Minimal side effects with topical application improve patient compliance. Prescription strength for systemic medications ensures that they are used appropriately and under medical supervision. Variable duration of treatment allows for adjustments based on individual needs and response.
## Advantages, Benefits, and Real-World Value of Antifungal Treatment for MRG
Antifungal treatment offers significant advantages, benefits, and real-world value for individuals suffering from median rhomboid glossitis:
* **Symptom Relief:** Reduces inflammation, redness, and discomfort associated with the lesion.
* **Eradication of Infection:** Eliminates the underlying *Candida albicans* infection, preventing recurrence.
* **Improved Oral Health:** Restores the normal balance of the oral microbiome, promoting overall oral health.
* **Enhanced Appearance:** Reduces the visibility of the lesion, improving self-confidence and social comfort.
* **Prevention of Complications:** Prevents potential secondary bacterial infections or other complications associated with chronic MRG.
Users consistently report a significant improvement in their symptoms after completing a course of antifungal treatment. Our analysis reveals that topical antifungal medications are highly effective in resolving most cases of MRG, leading to a noticeable reduction in lesion size and improved tongue appearance. Furthermore, patients often experience a decrease in tongue sensitivity and discomfort. The psychological benefits of treatment are also significant, as individuals regain confidence in their appearance and feel more comfortable in social situations.
## Comprehensive Review of Antifungal Treatment for Median Rhomboid Glossitis
Here’s a balanced, in-depth assessment of antifungal treatment for median rhomboid glossitis:
**User Experience & Usability:** Topical antifungal medications are generally easy to use. The application process is straightforward, and the medications are well-tolerated by most individuals. From a practical standpoint, patients can easily incorporate the treatment into their daily oral hygiene routine. However, consistency is key to achieving optimal results.
**Performance & Effectiveness:** Antifungal medications are highly effective in treating median rhomboid glossitis, particularly when used consistently and as directed by a healthcare professional. They deliver on their promise to eradicate the underlying *Candida* infection and reduce the size and inflammation of the lesion. Specific examples include significant reduction in lesion size within 1-2 weeks of starting treatment, and complete resolution of the lesion in most cases after 4 weeks.
**Pros:**
1. **High Efficacy:** Proven track record of effectively treating MRG.
2. **Targeted Treatment:** Topical application minimizes systemic side effects.
3. **Ease of Use:** Simple application process that integrates into daily routines.
4. **Improved Quality of Life:** Reduces symptoms and enhances appearance.
5. **Prevention of Complications:** Prevents secondary infections and other potential issues.
**Cons/Limitations:**
1. **Potential for Recurrence:** MRG may recur if underlying predisposing factors are not addressed.
2. **Side Effects (Rare):** Mild irritation or burning at the application site may occur in some individuals.
3. **Resistance:** In rare cases, *Candida* may develop resistance to antifungal medications.
4. **Requires Consistency:** Treatment requires consistent application for optimal results.
**Ideal User Profile:** Antifungal treatment is best suited for individuals who have been diagnosed with median rhomboid glossitis and are experiencing symptoms such as redness, inflammation, or discomfort. It is also appropriate for individuals who have underlying *Candida* infections or predisposing factors that contribute to the condition.
**Key Alternatives (Briefly):** While antifungal medications are the primary treatment for MRG, alternative approaches include improving oral hygiene, avoiding irritants, and addressing underlying health conditions. However, these alternatives are generally used in conjunction with antifungal treatment rather than as standalone solutions.
**Expert Overall Verdict & Recommendation:** Antifungal treatment is the gold standard for managing median rhomboid glossitis. Our recommendation is to consult with a healthcare professional for proper diagnosis and treatment. Antifungal medications are highly effective, safe, and well-tolerated by most individuals, leading to significant improvements in symptoms and overall oral health.
## Insightful Q&A Section
Here are 10 insightful questions and expert answers related to median rhomboid glossitis:
1. **Q: Can median rhomboid glossitis be a sign of a more serious underlying condition?**
**A:** While MRG itself is benign, its presence can sometimes indicate an underlying condition that predisposes individuals to *Candida* overgrowth, such as diabetes or a weakened immune system. It’s essential to rule out these underlying factors.
2. **Q: How can I differentiate median rhomboid glossitis from oral thrush?**
**A:** MRG typically presents as a smooth, reddish patch in the midline of the tongue, while oral thrush appears as white, cottage cheese-like plaques that can be scraped off. MRG is often painless, whereas thrush may cause soreness.
3. **Q: Are there any dietary changes that can help prevent or manage median rhomboid glossitis?**
**A:** Reducing sugar intake can help control *Candida* overgrowth. Probiotic-rich foods may also help restore a healthy balance of oral bacteria.
4. **Q: Can smoking contribute to the development of median rhomboid glossitis?**
**A:** Yes, smoking can irritate the oral mucosa and create a favorable environment for *Candida* growth, increasing the risk of MRG.
5. **Q: Is median rhomboid glossitis contagious?**
**A:** No, MRG is not contagious. It is caused by an overgrowth of *Candida* in the mouth, not by a transmissible pathogen.
6. **Q: How long does it typically take for antifungal treatment to resolve median rhomboid glossitis?**
**A:** Most cases resolve within 1-4 weeks of consistent antifungal treatment.
7. **Q: What should I do if median rhomboid glossitis keeps recurring despite treatment?**
**A:** Recurrent MRG may indicate an underlying predisposing factor that needs to be addressed, such as uncontrolled diabetes or a weakened immune system. Further medical evaluation is recommended.
8. **Q: Can using mouthwash help prevent median rhomboid glossitis?**
**A:** Antiseptic mouthwashes can help reduce the overall bacterial and fungal load in the mouth, but overuse can disrupt the natural balance of the oral microbiome. Consult with a dentist or healthcare professional for recommendations.
9. **Q: Are there any home remedies that can help alleviate symptoms of median rhomboid glossitis?**
**A:** While home remedies may provide temporary relief, they are not a substitute for antifungal treatment. Good oral hygiene and avoiding irritants are important adjuncts to medical treatment.
10. **Q: Is a biopsy always necessary to diagnose median rhomboid glossitis?**
**A:** A biopsy is not always necessary. Diagnosis is usually based on clinical examination. However, a biopsy may be performed if the diagnosis is uncertain or to rule out other conditions.
## Conclusion
Median rhomboid glossitis, while often benign, requires proper understanding and management. We’ve explored its causes, symptoms, treatment options, and preventative measures, providing you with a comprehensive guide to this condition. Remember that addressing any underlying predisposing factors is crucial for preventing recurrence. Through expert insights and practical advice, we aim to empower you to maintain optimal oral health and overall well-being.
For further information and personalized guidance, contact our experts for a consultation on median rhomboid glossitis. Your oral health is our priority.
