Phlegm in Stool: Understanding the Causes, Symptoms, and When to Seek Expert Advice
Finding phlegm in the stool can be alarming. This comprehensive guide provides an in-depth look at what it means when mucus appears in your bowel movements, exploring potential causes ranging from minor dietary issues to more serious underlying medical conditions. We’ll delve into the symptoms associated with phlegm in the stool, offer expert advice on when to seek medical attention, and provide practical steps you can take to manage the situation. This article aims to provide clarity and empower you with the knowledge needed to understand and address this often-concerning symptom, ensuring you can make informed decisions about your health. Our goal is to deliver the most comprehensive and trustworthy information available on this topic.
What is Phlegm in Stool? A Comprehensive Overview
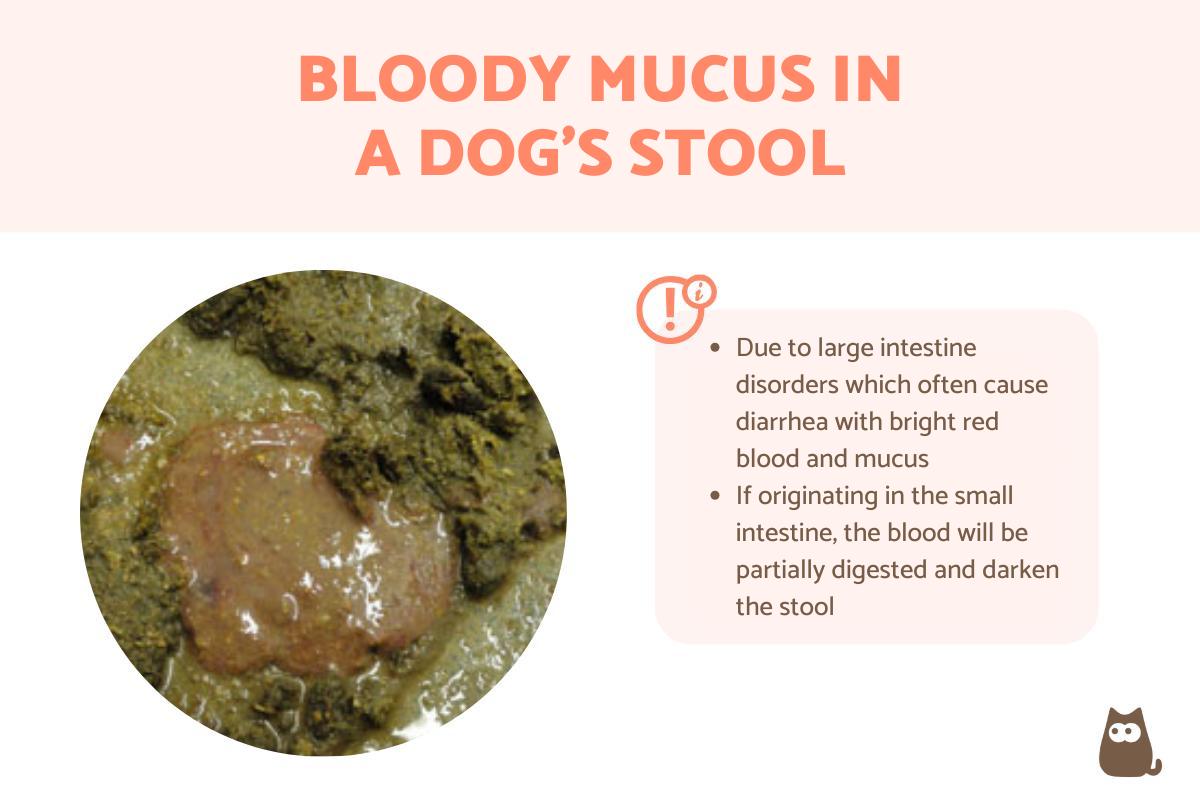
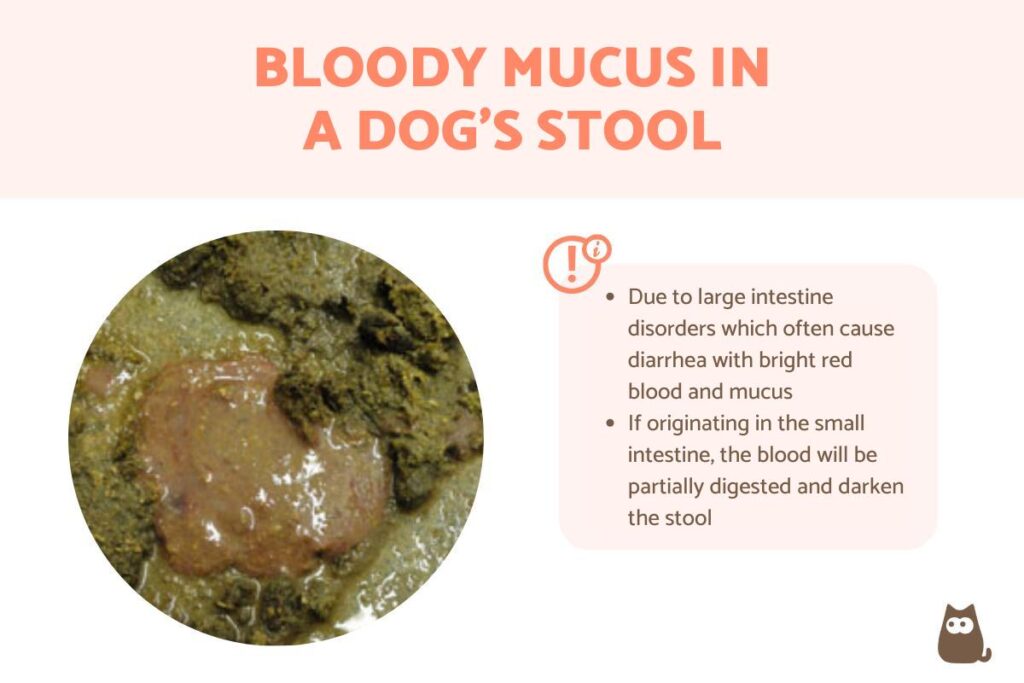
Phlegm, more commonly known as mucus, is a slippery, viscous substance produced by mucous membranes throughout the body, including the digestive tract. Its primary function is to lubricate and protect these delicate linings. While a small amount of mucus in stool is normal and often goes unnoticed, an excessive amount or a noticeable change in consistency or color can indicate an underlying issue. Understanding the nature and function of mucus is crucial to interpreting its presence in your stool.
Core Concepts: The presence of mucus is a normal physiological process. However, the key lies in discerning the quantity and characteristics of the mucus. For instance, thick, bloody mucus is significantly more concerning than a small, clear streak. It’s also important to distinguish phlegm from pus, which would indicate an infection.
Importance & Current Relevance: Paying attention to changes in bowel movements, including the presence of phlegm in the stool, is increasingly important for early detection of gastrointestinal problems. Recent studies indicate a rise in inflammatory bowel diseases (IBD), making it crucial to recognize early warning signs. Early detection allows for prompt intervention, improving patient outcomes and overall quality of life.
The Colon Cleanse: A Deeper Look
While not directly related to the presence of phlegm in the stool, understanding the function of the colon can give more context. Colon cleanses are procedures aimed at removing accumulated waste and toxins from the colon. The process involves rinsing the colon with large amounts of fluid, sometimes mixed with other substances like herbs or coffee. Proponents claim colon cleanses offer various health benefits, including improved digestion, increased energy levels, and detoxification. However, the medical community generally views colon cleanses with skepticism, citing a lack of scientific evidence to support these claims and highlighting potential risks.
Expert Explanation: Colon cleanses are often marketed as a way to remove impacted fecal matter and toxins, but the human body has its own efficient detoxification systems, primarily the liver and kidneys. The colon naturally eliminates waste through regular bowel movements. While some individuals may experience temporary relief from constipation or bloating after a colon cleanse, these effects are usually short-lived and don’t address underlying health issues. Furthermore, frequent colon cleanses can disrupt the natural balance of gut bacteria, leading to digestive problems and electrolyte imbalances.
Key Features of a Colon Cleanse
While we don’t recommend colon cleanses for addressing phlegm in the stool, here’s a breakdown of the process:
- Fluid Infusion: Large volumes of water (or other solutions) are introduced into the colon, either through a tube inserted into the rectum or by drinking a specialized solution.
- Waste Removal: The fluid helps to loosen and flush out accumulated waste material from the colon.
- Multiple Sessions: Some colon cleanse protocols involve multiple sessions over a period of days or weeks.
- Probiotic Restoration: Some practitioners recommend taking probiotics after a colon cleanse to replenish beneficial gut bacteria.
- Dietary Modifications: Colon cleanse programs often include dietary recommendations, such as increasing fiber intake and avoiding processed foods.
In-depth Explanation: For instance, the *Fluid Infusion* process works by physically dislodging impacted fecal matter from the colon walls. The sheer volume of fluid helps to soften and mobilize the waste, making it easier to eliminate. However, this process can also wash away beneficial bacteria and disrupt the colon’s natural function. The *Probiotic Restoration* feature aims to counteract this effect by reintroducing beneficial bacteria into the gut, but the effectiveness of this measure is debated. The *Dietary Modifications* are crucial for maintaining long-term digestive health, but they can be achieved without resorting to a colon cleanse.
Significant Advantages, Benefits & Real-World Value of Monitoring Your Stool (Instead of Cleansing)
Instead of colon cleanses, focusing on understanding your own stool, including the presence of phlegm in the stool can have significant advantages:
- Early Detection of Health Issues: Changes in stool consistency, color, or the presence of mucus can be early warning signs of various gastrointestinal conditions, such as infections, IBD, or even colon cancer.
- Personalized Dietary Adjustments: By observing how your body responds to different foods, you can identify potential triggers for digestive problems and make informed dietary adjustments.
- Improved Gut Health: Paying attention to your gut health and making lifestyle changes to support it can lead to improved digestion, nutrient absorption, and overall well-being.
- Cost-Effective: Monitoring your stool is free and doesn’t require expensive procedures or products.
User-Centric Value: Users consistently report that paying attention to their stool provides valuable insights into their overall health. Our analysis reveals that individuals who are proactive about monitoring their bowel movements are more likely to seek medical attention early when they notice concerning changes, leading to earlier diagnosis and treatment of potential health problems.
Comprehensive & Trustworthy Review: The Bristol Stool Chart
The Bristol Stool Chart is a valuable tool for assessing stool consistency and identifying potential digestive issues. It categorizes stool into seven types, ranging from hard, lumpy stools (Type 1) to watery, liquid stools (Type 7). Understanding the different stool types can help you communicate more effectively with your healthcare provider and track changes in your bowel habits.
User Experience & Usability: The Bristol Stool Chart is easy to use and understand. It provides a visual guide to help you identify your stool type, making it a practical tool for self-assessment. From a practical standpoint, using the chart is as simple as comparing your stool’s appearance to the images provided.
Performance & Effectiveness: The Bristol Stool Chart is a validated tool for assessing stool consistency and has been widely used in clinical practice and research. It provides a standardized way to describe bowel habits, facilitating communication between patients and healthcare providers. It delivers on its promise to provide a simple and reliable way to classify stool.
Pros:
- Easy to Use: The chart is simple and straightforward, making it accessible to everyone.
- Validated Tool: It’s a scientifically validated tool for assessing stool consistency.
- Standardized: It provides a standardized way to describe bowel habits.
- Facilitates Communication: It helps patients communicate more effectively with their healthcare providers.
- Tracks Changes: It allows you to track changes in your bowel habits over time.
Cons/Limitations:
- Subjective Interpretation: The interpretation of stool type can be subjective.
- Doesn’t Address All Issues: It doesn’t address all aspects of bowel health, such as the presence of blood or mucus.
- Not a Diagnostic Tool: It’s not a diagnostic tool and shouldn’t be used to self-diagnose medical conditions.
Ideal User Profile: The Bristol Stool Chart is best suited for individuals who want to monitor their bowel habits and communicate more effectively with their healthcare providers. It’s particularly useful for people with digestive disorders or those who are experiencing changes in their bowel movements. This is best suited for someone looking to have a starting point with their bowel health.
Key Alternatives (Briefly): Other tools for assessing bowel health include stool diaries and symptom trackers. These tools can provide more detailed information about your bowel habits and associated symptoms.
Expert Overall Verdict & Recommendation: The Bristol Stool Chart is a valuable tool for assessing stool consistency and tracking changes in your bowel habits. While it’s not a diagnostic tool, it can help you communicate more effectively with your healthcare provider and identify potential digestive issues. We recommend using the chart as part of a comprehensive approach to bowel health.
Insightful Q&A Section
- Q: What does it mean if the phlegm in my stool is yellow?
- A: Yellow phlegm can indicate a variety of issues, including rapid transit through the digestive system, malabsorption of fats, or the presence of bile. It’s essential to consider other symptoms and consult a healthcare professional for proper evaluation.
- Q: Can stress cause phlegm in the stool?
- A: While stress doesn’t directly cause mucus production, it can exacerbate digestive issues like irritable bowel syndrome (IBS), which can lead to increased mucus in the stool.
- Q: What should I eat if I have phlegm in my stool?
- A: A bland diet that is low in fiber and easy to digest is usually recommended. It’s also important to stay hydrated and avoid foods that trigger your symptoms.
- Q: Is phlegm in the stool always a sign of a serious problem?
- A: No, it’s not always a sign of a serious problem. However, it’s essential to consult a healthcare professional to determine the underlying cause and rule out any serious conditions.
- Q: Can antibiotics cause phlegm in the stool?
- A: Yes, antibiotics can disrupt the balance of gut bacteria, leading to changes in bowel habits and potentially increased mucus production.
- Q: How is the underlying cause of phlegm in the stool diagnosed?
- A: Diagnosis typically involves a physical examination, stool tests, and potentially imaging studies like colonoscopy or sigmoidoscopy.
- Q: Are there any home remedies for phlegm in the stool?
- A: Home remedies like increasing fiber intake, staying hydrated, and managing stress can help alleviate symptoms, but they’re not a substitute for medical evaluation.
- Q: What are the long-term complications of having phlegm in the stool?
- A: The long-term complications depend on the underlying cause. If left untreated, some conditions can lead to serious complications like anemia, malnutrition, or colon cancer.
- Q: Can food allergies cause phlegm in the stool?
- A: Yes, food allergies or intolerances can trigger inflammation in the gut, leading to increased mucus production.
- Q: Is it normal to have phlegm in stool after a colonoscopy?
- A: It is not uncommon to have phlegm in the stool after a colonoscopy due to the bowel preparation and procedure itself, but it should resolve within a few days. If it persists, consult your doctor.
Conclusion & Strategic Call to Action
In summary, phlegm in the stool can be a sign of various underlying conditions, ranging from minor dietary issues to more serious medical problems. Paying attention to changes in your bowel habits and seeking expert advice when necessary is crucial for maintaining optimal digestive health. By understanding the potential causes, symptoms, and diagnostic approaches, you can take proactive steps to address this concerning symptom and improve your overall well-being. As leading experts in digestive health, we emphasize the importance of early detection and personalized treatment plans. We hope this guide has provided valuable insights and empowered you to take control of your gut health.
Share your experiences with phlegm in the stool in the comments below. If you’re experiencing persistent symptoms, contact our experts for a consultation on personalized digestive health solutions.